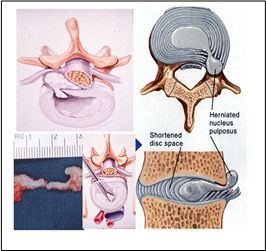
When the nucleus pulposus from the intervertebral disc escapes from its normal anatomical confines, it can irritate the adjacent nerve root, causing the typical radiculopathy pain. It is a common cause of back pain and sciatica. Besides direct mechanical compression, the nucleus pulposus itself is also a biologically active tissue and may induce significant inflammation, causing nerve root symptoms. The type of herniation could be defined by its relationship with the annulus and the posterior longitudinal ligament (PLL), which can be a contained budging disc, an extruded disc, or a sequestrated disc.
Treatment of Prolapsed Intervertebral Disc
Symptoms of prolapsed intervertebral disc may improve after conservative treatment. 50% of the cases would have their pain improved in a few weeks.
The indications for surgical intervention include patients with neurological complications (e.g. cauda equina syndrome), patients with symptoms not responding to conservative treatment, and patients with significant and progressive neurological deficit. Relative indications for surgery would be patients with recurrent and significant relapse of symptoms.
Surgery aims to decompress the compressed nerve root. This can be achieved by a discectomy through open surgery, or with minimally invasive technique. At the same time, we should also consider if there is any back pain symptoms that may be related to the instability of the diseased intervertebral disc. If there is significant back pain related to instability, a fusion surgery, either through an anterior or posterior approach, would be indicated to remove the instability factor causing the back pain.